Conventionally, healthcare has been perceived as a vocation. A potentially lucrative one, yes, but founded on the core principles of service and dedication toward the community.
In modern times, these pillars remain more relevant than ever. A Gallup trust survey found that more than 75% of people trust nurses, holding them to high ethical standards. About 53% trust doctors, showing some degree of apprehension but still revealing trust levels higher than those we place in many other professions.
Undoubtedly, healthcare recruiters must continue to prioritize skills like a willingness to serve and transparency in communication. However, they must also look for competencies that go beyond these traditional expectations.
Candidates with the below skillsets can deliver a higher performance that improves health outcomes for the people and families they serve.
1. Ethical, Not Just Critical, Problem-Solving
Critical thinking has a spot on most recruiter lists today when it comes to soft skills, with some demanding that candidates demonstrate it through past projects or experiences. Admittedly, critical thinking is essential for healthcare workers to make decisions that help their patients achieve better outcomes.
The oversight we sometimes make is forgetting to encompass ethical priorities when assessing this competency.
The healthcare sector is replete with ethical quandaries, many of which practitioners face frequently on the job. Research studies indicate that the COVID-19 pandemic exposed deep-rooted problems in many organizations in this sector. Professionals and clients report experiencing emotional overload and institutional betrayal.
With many services now digitalized, the possibility of ethical dilemmas is even higher. A study published in Frontiers in Human Dynamics observes that the ability to access mental health online has increased ethical risks. From data breaches and misuse of information to incorrect diagnoses and their repercussions, the challenges are numerous.
Only an ethically sound professional who knows how to make tough decisions without losing moral agency can thrive in such circumstances. Recruiters can assess a candidate’s readiness for the job by discussing scenarios that test ethical problem-solving skills.
For example, would they prioritize patient care and safety or the patient’s free will to deny treatment? How would they facilitate healthcare access to socially or economically marginalized communities? Depending on the role you are hiring for, you can converse about pharmacological, administrative, or therapeutic subjects.
2. Interdisciplinary Collaboration
Why should patients be deprived of better health results just because an organization lacks staff with collaboration capabilities?
For instance, rehabilitation teams for stroke survivors are increasingly becoming multidisciplinary. They often comprise doctors, nurses, physiotherapists, and mental health professionals. A 2025 Frontiers in Neurology study found that interdisciplinary interventions and personalized assessments can improve motivation among patients and remove barriers to care.
Being unable to work harmoniously and productively in such interdisciplinary teams can prove to be a significant shortcoming in otherwise capable candidates.
The rising demand for this skill has encouraged academicians to take note. Some universities have started integrating a strong sense of community into the curriculum for courses like a master of science in nursing. This helps future professionals learn to connect with experts, peers, and other stakeholders during their practice.
Felician University emphasizes the role of real-world experiences and hands-on training through clinical opportunities. These opportunities can help professionals be well-prepared for future roles in their selected specialty area in healthcare.
The best part is that prioritizing this skillset also brings along several other core competencies, such as emotional intelligence and conflict management. When you work in a team that spans specialties, roles, and seniorities, these soft skills are essential to deliver patient-centric care.
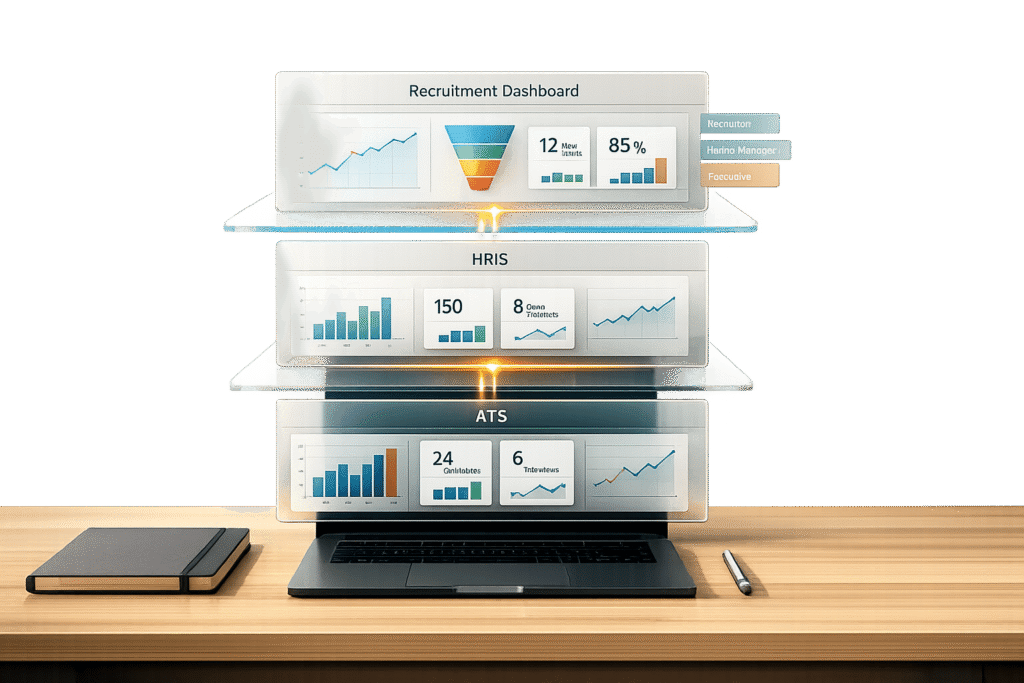
3. Familiarity and Keenness Toward Healthcare Tech
Imagine a scenario in which a hospital wants to roll out new software for nursing administration. The goal is to streamline tasks for the nursing staff, thereby freeing up more time for patient-focused activities. A tech-averse nurse manager or leader is unlikely to embrace this change with enthusiasm.
Healthcare technologies are growing rapidly, from telemedicine to AI tools for precise diagnostics. McKinsey’s 2026 health outlook stresses the rise of agentic AI and ambient listening, among other technologies that promote healthcare access and affordability. The impact of these interventions has been so phenomenal that it is highly unlikely the ‘wave’ will die out anytime soon.
During interviews, check whether the candidate is familiar with and shows eagerness toward healthcare technologies. You can also judge their interest levels by the courses they have pursued or seminars they have attended for new technologies, such as IoT and wearable devices. Continuous learning becomes more than a concept only when one can demonstrate their endeavors in this direction.
The Bottomline
Contemporary recruitment drives for healthcare roles are different from their older counterparts. The emphasis on team dynamics, collaboration, and technology is pronounced, in keeping with a changing world.
Healthcare recruiters can benefit from seeking these new-age skills in potential recruits to build a more capable workforce.
Author bio: Writer by day, dream catcher by night. Marchelle Abrahams cut her teeth during the infancy of the internet when the dial sound of the modem was more than a soundbite at a rave. Not a Millennial and not a Boomer, Marchelle is an in-betweener, making her a special breed of human. As a qualified journalist, Marchelle believes her superpower is stringing a few words together and people reading them.